A recent study has revealed that infection with the widely prevalent parasite Toxoplasma gondii can significantly impair brain function in intermediate hosts, with possible implications for humans. This disruption occurs even with a limited number of neurons affected by the parasitic infection, highlighting the profound impact that T. gondii can have on neuronal communication.
The research, conducted by scientists at the University of California Riverside School of Medicine, involved the examination of mouse brain cells, both cultured in vitro and taken directly from live animals. Results indicated that neurons infected with T. gondii produced fewer extracellular vesicles (EVs)—tiny lipid-bound packets that facilitate intercellular communication. These findings are critical, as they contribute to the ongoing debate regarding the behavioral effects of toxoplasmosis.
Emma Wilson, a parasite immunologist involved in the study, explained, “We found this disruption in EV signaling can interfere with how neurons and glial cells, especially astrocytes, maintain a healthy brain environment. Even a handful of infected neurons can shift the brain’s neurochemical balance, suggesting that neuron-glial communication is both vital and susceptible to parasitic influence.”
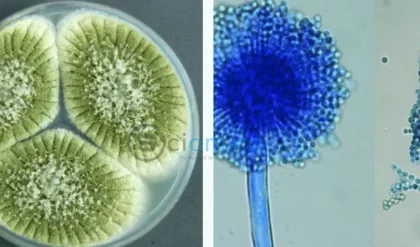
T. gondii is notorious for instigating behavioral changes in its hosts, which can be either beneficial or detrimental. The parasite prefers to infiltrate neurons, crossing the blood-brain barrier and potentially residing within the host’s body for decades. It is one of the most successful parasites worldwide, capable of invading a myriad of warm-blooded species, yet it can only reproduce in cats. Research has indicated that some of the behavioral alterations manifested in infected organisms are designed to enhance the likelihood of encounters with cats, leading, for instance, to rodents being attracted to the smell of cat urine rather than avoiding it.
While some studies point to circumstantial evidence for these behavioral manipulations, establishing definitive links to the parasite’s influence is complex, especially in humans where behaviors are influenced by myriad factors.
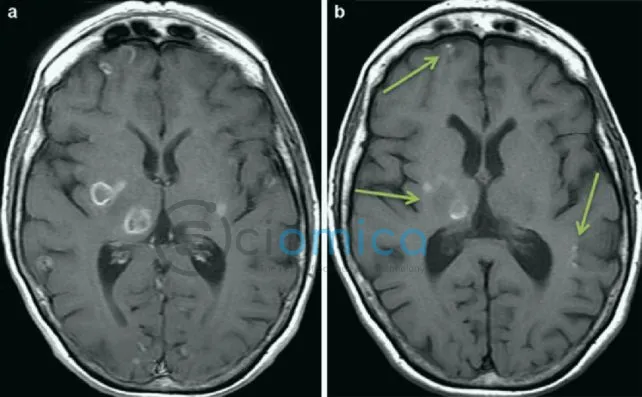
The recent research does not delve into behavioral outcomes; rather, it focuses on the physiological evidence of parasite effects. By infecting mouse neurons and analyzing EV production, the team discovered a marked reduction in EV generation and alterations in their content compared to healthy neurons. These changes had significant repercussions on astrocyte gene expression, prompting specific immune responses while diminishing the efficacy of glutamate transporters—known for mitigating excess glutamate levels in the brain.
Excess glutamate is associated with serious neurological problems, including seizures and neural damage, known consequences of severe toxoplasmosis. This suggests that the impact of T. gondii on human health may be underestimated.
With an astonishing number of people harboring T. gondii, primarily acquired from undercooked food or contact with cat feces, prevalence rates can soar to 80% in certain regions and hit 10-30% in the U.S. Most individuals remain blissfully unaware of their silent parasitic companions, but vulnerable groups—namely infants, the elderly, pregnant women, and those with compromised immune systems—face heightened risks.
The study underscores the necessity of preventive measures such as thorough cooking of meat, washing vegetables, and maintaining hygiene after handling cat litter. Wilson asserts that understanding the interplay between the immune response and the parasite could lead to better protective strategies for at-risk individuals.
As this field of research progresses, insights like these could significantly reshape our understanding of neurological health and the implications of parasitic infections.
The findings have been published in PLOS Pathogens.